About
Adverse Drug Reactions
Adverse drug reactions (ADRs) are the unintended responses or harmful side effects (expected or unexpected) caused by the normal dose of a drug. ADRs are among the top ten causes of all deaths in North America. Many of these ADRs are caused by inherited genetic differences.
The annual cost of ADRs has been estimated to be over $13 billion in Canada. This is likely an underestimation, since 95% of ADRs are not reported to health regulators. Even if only the most severe ADRs are considered, there are an estimated 200,000 ADRs each year in Canada resulting in hospital admission and causing tens of thousands of deaths.
Examples of Adverse Drug Reactions
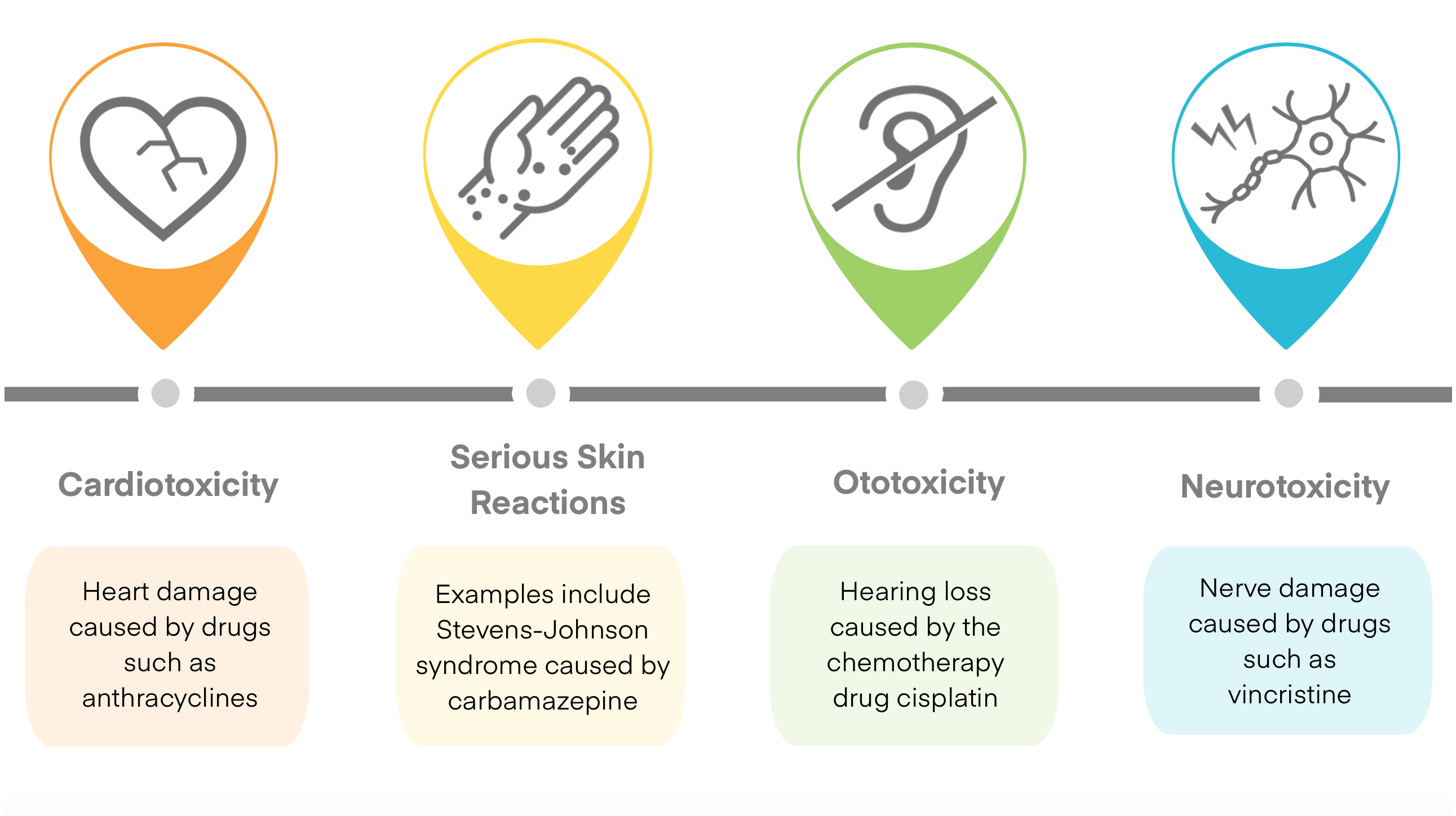
While drugs are tested in clinical trials to show that they are safe and efficacious for the general population, they do not adequately account for variations in drug response between all individuals. The same dose of one drug may be effective in one individual, but can cause a severe ADR in another.
There are a variety of factors known to influence the variability in drug effects seen in real-world populations. These include a patient’s age, sex, ancestry, use of concomitant medications, weight, diet, adherence to therapy, and concomitant diseases. Genetic variation, specifically genetic polymorphisms in drug biotransformation genes, is a key factor in the occurrence of serious ADRs. The study of the contribution of genetics to drug response is referred to as pharmacogenomics.
The CPNDS aims to develop pharmacogenomic tests to predict whether patients will develop severe ADRs. This information can be used to adjust an individual’s dosage, choose an alternative drug, or monitor drug response more closely. The process of tailoring treatment to groups or individual patients is referred to as precision medicine.
Towards Precision Medicine
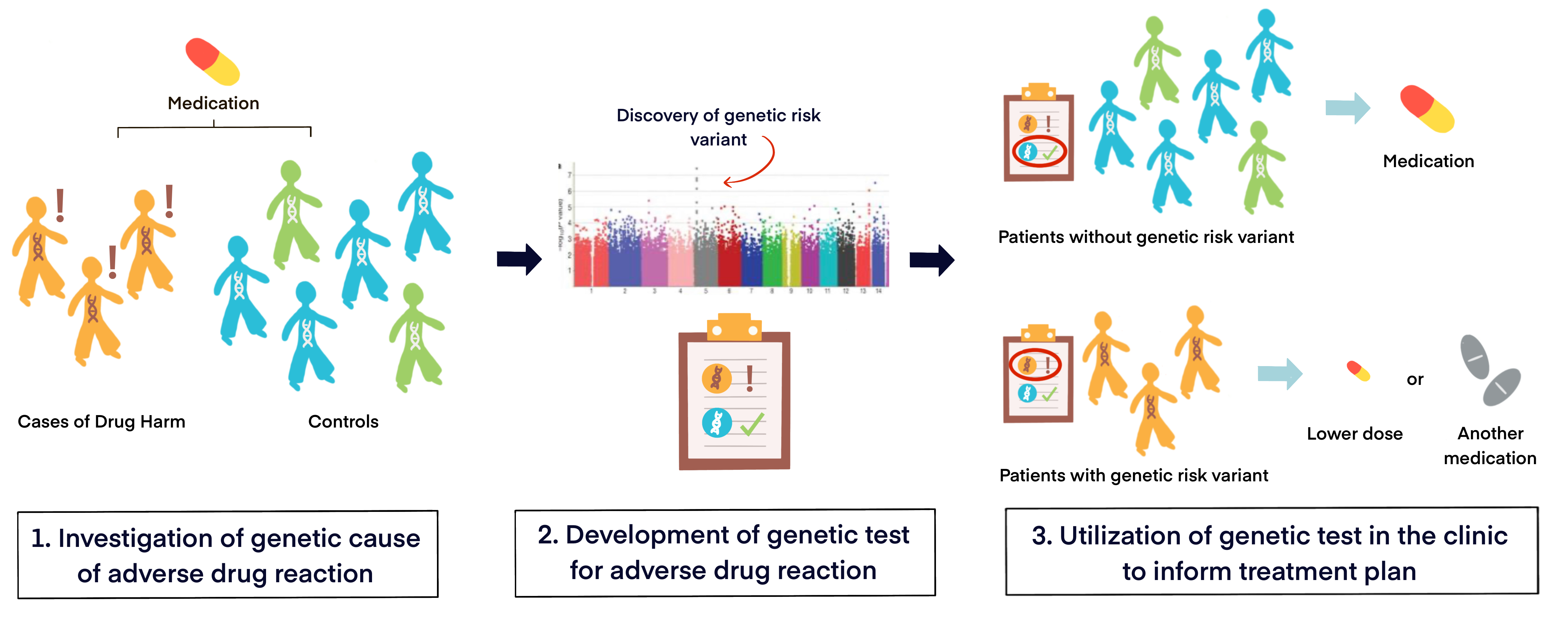
The Genetic Cause of ADRs
To uncover the genetic cause of ADRs, we look for patients in two groups:
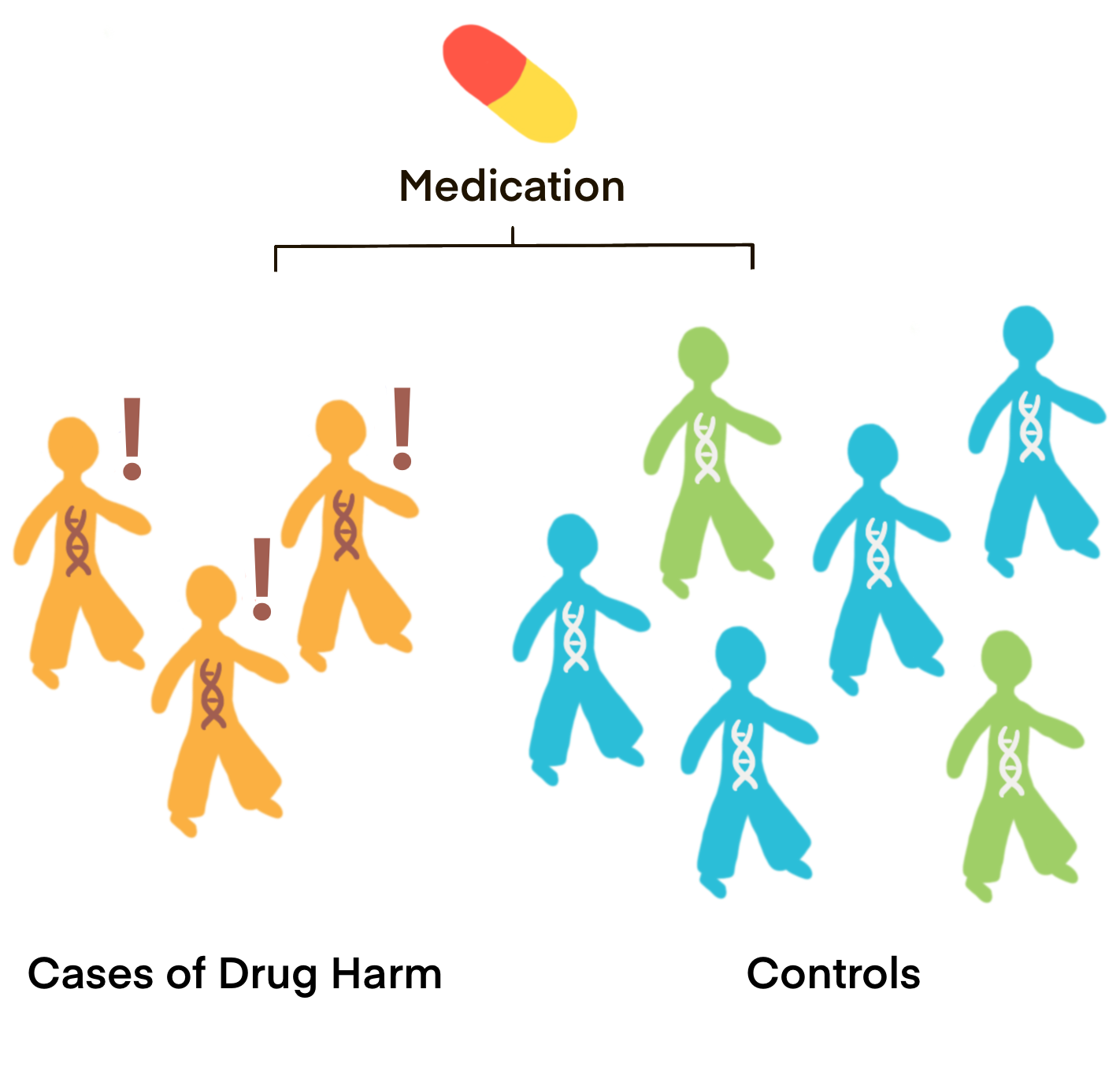
1) Cases: Patients who took a drug and developed an ADR
2) Controls: Patients who took the same drug but did not develop the ADR under study
We collect DNA samples (blood or saliva) and clinical information from all patients, including information about reactions from cases. This allows us to look at genetic and clinical differences between cases and controls.
Computational biological analyses are conducted to find genetic variants that appear significantly more frequently in patients with ADRs. If these genetic variants are strongly linked to the development of an ADR, and once these findings are replicated and validated, they can be used as a diagnostic test to predict the ADR. To understand the generalizability of the findings, this process is replicated in different populations.
The Active Surveillance Network
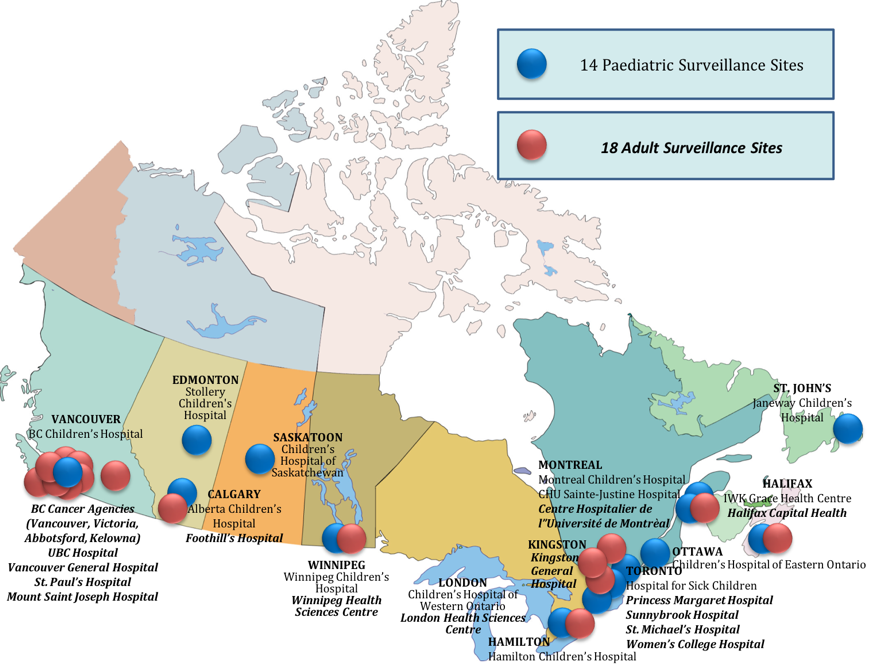
The CPNDS has developed a Canada-wide active surveillance network which searches for patients with ADRs. Active ADR surveillance provides a system that overcomes many of the shortcomings of voluntary ADR reporting. In the active surveillance network described here, trained surveillance clinicians, whose sole responsibility it is to identify and report ADRs, provide both the expertise and are ensured the dedicated time required to obtain detailed drug safety information.
In order to comprehensively assess the safety profile of a drug, nationwide surveillance and collection of clinical data on ADRs from multiple healthcare institutions is needed. An active ADR surveillance network can provide the necessary framework to coordinate data collection in a standardized manner, facilitating the interrogation of clinical data to determine factors that contribute to the risk of an ADR. Similarly, such a network, through its direct link to healthcare professionals in their respective institutions (e.g. hospitals, academic health centres, clinics), enables a coordinated and efficient communication of drug risk evaluation results to clinicians for a rapid uptake of safety alerts in clinical practice.
Moreover, active surveillance can capture ADRs across the entire population of patients exposed to drugs in a variety of clinical settings, and is thus able to inform health authorities on true drug risks in everyday clinical practice. At the same time, an active surveillance system allows targeted recruitment and follow-up of patients focused on a specific ADR, a specific drug, or a specific patient subpopulation (e.g. age groups, ethnic groups, gender). With such targeted investigations, relevant information on a specific drug safety question can be obtained very efficiently and within a relatively short time. Most importantly, active surveillance provides a means to evaluate drug safety particularly in populations often excluded from clinical trials, such as children and pregnant women.
Of equal importance, active surveillance by trained clinicians enables the collection of standardized, detailed and high-quality ADR reports, which are critical for the evaluation of drug risk. With detailed and high-quality clinical data, thorough analyses of factors that increase the susceptibility of a patient to suffer from an ADR, are possible. The identification of susceptibility factors and those individuals at greatest risk for ADRs is key to an improved overall drug safety. Once such susceptibility factors are identified, this information can be incorporated into drug labels and clinical practice guidelines to inform clinicians about an increased drug risk in specific patient subpopulations, and thus contribute to better-informed clinical decision making through stratification of patients according to their risk of developing a specific ADR, reducing the occurrence of serious and life-threatening ADRs.
The CPNDS Database
In addition to its network infrastructure of active surveillance clinicians and scientists, the CPNDS maintains a database with extensive longitudinal phenotypic data including medication history, laboratory results, and description of ADRs with clinical and temporal details. The CPNDS has been established for more than 16 years as of 2021. Data has been collected for some patients since inception.
All patient data files can be updated as needed over time; this is a key advantage of observational data collected through an active surveillance network.
Based on data collected between May 15, 2005, and May 9, 2017, there have been 93,974 reports of medication use, 10,475 of which are ADR cases, and 83,499 of which are non-ADR reports. The cases are comprised of similar numbers of male and female patients, but are mostly pediatric patients (72.6%), which reflects the network’s focus on pediatric ADRs, particularly in cancer treatment where potent pharmacological agents are used at high doses to prolong life, thereby increasing the occurrence of serious ADRs. Self-reported ancestry varies among study participants, but are most commonly European (38.2%), Canadian (9.6%), and East Asian (4.9%). Serious cutaneous reactions are the most commonly described ADR in the database, followed by peripheral neuropathy and cardiotoxicity. The reactions were induced by a variety of drugs, including chemotherapeutics, antibiotics, and antiviral medication.
Our Research
Progress
The CPNDS has identified genetic variants that play a role in cisplatin-induced hearing loss, anthracycline-induced cardiotoxicity, and opioid- and vincristine-induced toxicities.
Projects
We are currently using our findings to develop pharmacogenetic tests, validate mechanisms of drug response variation, and develop novel adverse drug reaction targets.
Publications
Learn more about our group’s select publications in areas such as drug-induced skin reactions, machine learning and big data, and clinical practice guidelines.